With June flying by and summer truly underway, it’s the perfect time to encourage your little ones to embrace the outdoors and learn a new skill that promotes both physical activity and independence–bicycle riding. Bike riding is not only a great summer pastime but also a fantastic way to enhance your child’s balance, coordination, strength, and overall motor skills!Choosing the Right Bike: Pedal Bike with Training Wheels vs. Balance Bike When it comes to teaching children how to ride, parents often debate between pedal bikes with training wheels and balance bikes. Each option has its unique benefits as described below: Pedal bikes with training wheels provide immediate stability, helping children feel secure as they learn to pedal. However, they can sometimes inhibit the development of balance and coordination. Balance bikes—bicycles without pedals—focus on teaching children to balance first, often leading to quicker mastery of biking skills and a smoother transition to pedal bikes without the need for training wheels. However, some children have difficulty propelling themselves forward while sitting and balancing. It is possible to modify a bike with training wheels to be utilized more similarly to a balance bike by; and there are also some models of balance bikes which allow you to add pedals later on! To modify a pedal bike:
Choosing the Right Time to Start The ideal time to teach your child to ride a bike varies, most typically between ages 3 and 6. Look for signs of interest and readiness such as curiosity about bikes and a willingness to try new activities. Your little one should have the strength to pedal a bike prior to utilizing a pedal bike, and if that is not the case a balance bike may be a better option! Ensuring Safety First Safety is paramount when teaching your child to ride a bike. Choose a safe, flat location away from traffic. Ensure your child wears a properly fitted helmet and comfortable clothing. And teach them the basic rules of the road. Correctly Sizing the Bike Proper bike sizing is crucial for comfort and safety: Your child should be able to stand over the top tube with feet flat on the ground and have about 1 to 3 inches of clearance. Adjust the seat height so they can comfortably reach the pedals with a slight knee bend when fully extended. Avoid getting a bike that is too large in hopes of having them grow into it, as it can be harder for them to control. Teaching your child to ride a bike is a memorable milestone that promotes physical health and independence. Whether you choose a pedal bike with training wheels or a balance bike for your little one, prioritize safety and ensure the bike is correctly sized. With patience, encouragement, and the right guidance, your child will soon be biking confidently towards new adventures this summer and beyond.
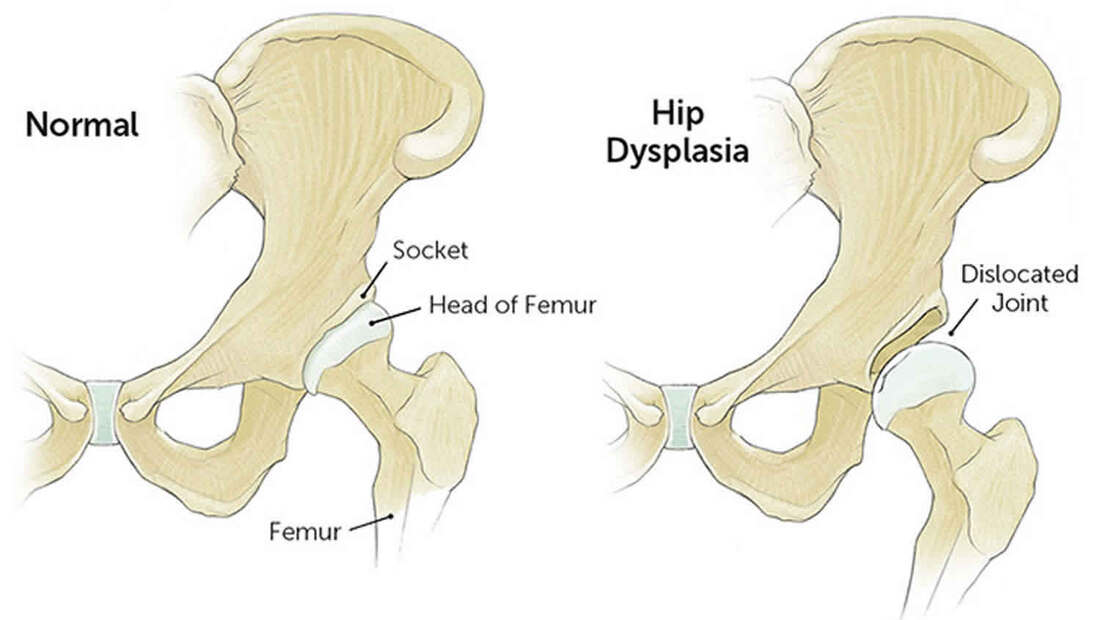
At Leaps and Bounds PT, we support your child’s development with personalized guidance on motor skill development. Consult your child’s physical therapist for expert advice tailored to your child’s needs, especially if you have concerns regarding their physical milestones or readiness leading up to bike riding. Stay active, stay safe, and enjoy the ride this summer! As the warm weather rolls in, parents of new walkers are eager to explore outdoor activities with their little ones. Summer presents a perfect opportunity to engage in activities that not only entertain, but also support the development of their child's newfound walking skills. Leaps and Bounds emphasizes the importance of movement and exploration in early childhood development. Here, Dr. Lindsey has curated a list of summer activities tailored specifically for new walkers to enhance their motor skills while having a blast under the sun!1. Nature Scavenger Hunt: Embark on a nature scavenger hunt in your local park or neighborhood. Create a simple list of items for your child to find, such as leaves, flowers, rocks, or sticks. Encourage them to walk independently as they search for each item. This activity not only promotes walking but also enhances observation skills and fosters a connection with the natural world. 2. Water Play: Summer and water activities go hand in hand. Fill a small kiddie pool or water table with shallow water and let your new walker splash and play. Place floating toys or objects slightly out of reach to encourage them to take steps and reach for them. Walking in water provides resistance, which strengthens muscles and improves balance. Just remember, safety first—always supervise your child around water, no matter how shallow. 3. Sensory Walks: Take your little explorer on a sensory adventure through nature. Parks, beaches, and even your backyard offer various textures, temperatures, and surfaces to stimulate their senses. Encourage your child to feel the grass under their feet, the sand between their toes, and the cool water as they splash around. Sensory experiences like these help improve balance, coordination, and proprioception. 4. Outdoor Music and Dance: Put on some lively music and groove together in the backyard or local park. Encourage your child to move to the beat, taking steps and exploring different movements. Dancing helps improve motor planning, rhythm, and coordination. Plus, it's a fantastic way to bond and have fun together as a family. 5. Miniature Golf: Miniature golf courses offer a perfect setting for new walkers to practice their skills in a structured environment. The gentle slopes, ramps, and obstacles provide opportunities to develop balance, coordination, and spatial awareness. Guide your child as they navigate through the course, celebrating each successful putt and step they take. 6. Sidewalk Chalk Art: Unleash your child's creativity while promoting physical activity with sidewalk chalk art. Let them explore their artistic side by drawing shapes, lines, and squiggles on the pavement. Encourage them to walk around as they draw, practicing balance and coordination. You can even create a mini obstacle course or hopscotch to add an extra element of fun and challenge. Summer is a season of exploration, growth, and fun for new walkers. By engaging in these outdoor activities, parents can support their child's physical development while creating cherished memories together. Remember to always prioritize safety, provide encouragement, and celebrate every milestone along the way. With each step taken and every adventure embarked upon, your little one is not only exploring the world but also building a strong foundation for a lifetime of movement and discovery!Pediatric hip dysplasia is a complex condition that can affect infants, children, and adolescents, with significant implications for long-term musculoskeletal health. In this blog post, Dr. Brianna aims to shed light on this condition, discussing its causes, diagnosis, treatment options, and the latest research advancements.What is Pediatric Hip Dysplasia? Pediatric hip dysplasia, also known as developmental dysplasia of the hip (DDH), refers to an abnormal development of the hip joint. It can range from mild instability to complete dislocation of the hip joint. DDH can occur during fetal development, infancy, childhood, or adolescence, and its severity varies among individuals. What causes hip dysplasia? The exact cause of pediatric hip dysplasia is not always clear, but several factors can contribute to its development. These include genetics, breech position during pregnancy, swaddling or tight wrapping of infants' hips, and certain environmental factors. Female infants are more prone to DDH than males, and it often runs in families. How is hip dysplasia diagnosed? Early detection of hip dysplasia is crucial for effective management and preventing long-term complications. Newborns are routinely screened for hip dysplasia using physical examination techniques like the Ortolani and Barlow tests. Imaging studies such as ultrasound or X-rays may be used for confirmation if the physical exam is inconclusive. In older children and adolescents, clinical symptoms like limping, leg length discrepancy, or hip pain may prompt further evaluation with imaging studies. What is the proper treatment for hip dysplasia? Treatment strategies for pediatric hip dysplasia depend on the age of the child and the severity of the condition. In infants, gentle manipulation and positioning techniques like Pavlik harness or Frejka pillow may be used to maintain proper hip alignment and promote normal joint development. For older children and adolescents, treatment may involve bracing, stretching, therapeutic exercise, or surgical interventions. Have there been any advances in research regarding hip dysplasia? Recent research in the field of pediatric orthopedics has focused on improving diagnostic techniques, refining treatment algorithms, and understanding the long-term outcomes of hip dysplasia management. Advances in imaging technology, such as three-dimensional ultrasound and magnetic resonance imaging (MRI), offer better visualization of hip anatomy and aid in early diagnosis. Moreover, studies exploring the genetic basis of DDH provide insights into its underlying mechanisms and potential targets for future therapies. Longitudinal cohort studies tracking patients from infancy to adulthood help evaluate the effectiveness of different treatment modalities and identify factors influencing outcomes, such as age at diagnosis, severity of dysplasia, and compliance with treatment protocols. Conclusion: Pediatric hip dysplasia is a multifaceted condition that requires early detection and tailored management approaches to optimize outcomes. Through ongoing research efforts and multidisciplinary collaboration, healthcare professionals aim to enhance our understanding of DDH, refine treatment strategies, and improve the quality of life for affected individuals from infancy through adolescence and beyond.
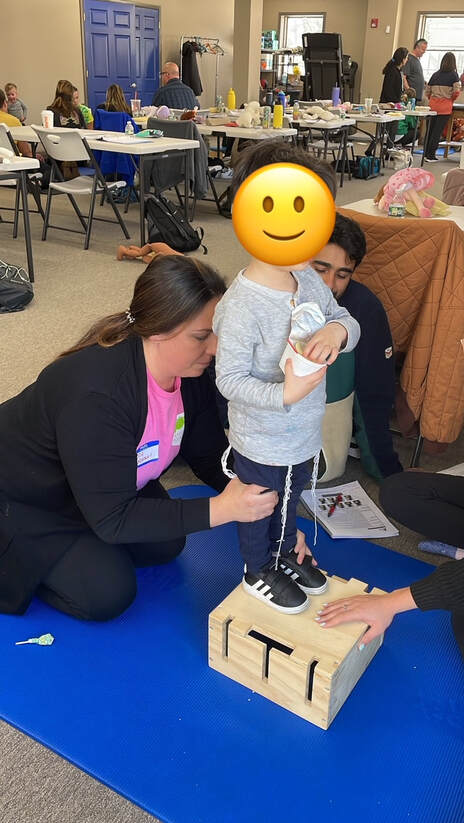
As the weather gets warmer, and days grow longer, we also step into a very special time of the year, Autism Acceptance Month! The Spring season, symbolic of growth, offers a perfect backdrop to highlight the journey of children with autism, especially through the lens of physical therapy. Join Dr. Bassem as we celebrate these incredible children and the unique benefits that physical therapy can bring to their lives. As a pediatric physical therapist, I've had the privilege of witnessing firsthand the remarkable strides children with autism can make when supported with compassion, understanding, and personalized care. Physical therapy plays a pivotal role in the development of children with autism by encouraging motor skills, while also fostering a sense of independence, confidence, and engagement with the world. Children with autism often face challenges with gross motor skills such as walking, running, or jumping. They may also struggle with fine motor skills, including grasping objects or performing delicate tasks. Yet, with personalized exercises and activities, we can nurture the development of these skills in a comfortable and conducive environment. Through active listening, empathy, and patience, the therapist can adapt their approach to suit the child's communication style, whether it involves verbal language, nonverbal cues, or alternative communication methods. Spring also brings a symphony of sensory experiences, from the scent of flowers to the feel of grass underfoot. Similarly, physical therapy can help children with autism navigate their sensory experiences more effectively. Through controlled exposure to various physical stimuli in a safe environment, therapy can help reduce sensory sensitivities and improve sensory processing, making the world a less overwhelming place. Physical therapy sets the stage for children with autism to achieve greater independence. By improving motor skills and coordination including running, jumping, throwing & kicking a ball, children can gain the ability to perform daily activities with less assistance. This April, as we watch the world around us burst into life, let's also celebrate every step, jump, and milestone achieved by children with autism. Their journey is a testament to the resilience and potential within each of them, waiting to blossom with the right support and nurturing. By advocating for inclusive environments and supporting therapies that cater to the unique needs of children with autism, we contribute to a world where every child can thrive. The journey with autism, much like the unfolding of Spring, is filled with moments of growth and discovery. Celebrate differences and let us make Autism Acceptance Month a time of joyful celebration and commitment to acceptance! One of our main goals at Leaps and Bounds Pediatric Physical Therapy is to aid our children and families through education and by fostering a community. One of our newest class offerings at our Holmdel, NJ location aims to do just that- read on as Dr. Lindsey talks about our new addition: Baby Bootcamp! What is Baby Bootcamp? Baby Bootcamp is a class designed for new and expectant parents to learn about the Motor Milestones their baby will achieve from birth to 18 months. Within the class we cover skills such as rolling, crawling and walking, and so much more! This class combines both education and purposeful play by having parents actively participate in helping their baby practice these skills with the help of Dr. Lindsey and Dr. Leandra. Throughout the course we provide not only different activities to use with your child, but recommendations for age-appropriate toys as they grow. Who is right for Baby Bootcamp? Baby Bootcamp is broken up into 2 groups based on age and current skill level:
How do I sign up for Baby Bootcamp? The link to sign up for Baby Bootcamp is provided below, also available on our website and Instagram page @leapsandboundspt. Classes can either be purchased individually or in a pack of 3. Included in the purchase of a pack of 3 is the opportunity to email our Physical Therapists with questions you may have concerning your baby in between classes! Our Spring Schedule is as Follows: Friday 3/29: 11am Rockers and Rollers, 12pm Movers and Groovers Friday 4/26: 11am Rockers and Rollers, 12pm Movers and Groovers Friday 5/17: 11am Rockers and Rollers, 12pm Movers and Groovers For any questions, please feel free to email [email protected] or call our Holmdel location at (732)-479-2472.
We look forward to seeing you and your baby there! To sign up for this class, please visit our classes page and click the image to get started! Classes - Leaps and Bounds PT LEAPING into The LEAP Year: Proper Mechanics and Red Flags for Jumping in the Pediatric Population2/1/2024
Jumping is not only a fundamental movement skill but also a joyful activity for children. From hopscotch to basketball, mastering proper jumping mechanics is essential for both performance and injury prevention in pediatric populations. In this blog, Dr. Brianna will delve into the importance of correct jumping form for children and highlight red flags to watch out for, indicating improper mechanics.Why Proper Jumping Mechanics Matter Jumping involves coordinated movement of various muscles and joints, making it a complex skill to master. For pediatric populations, learning proper jumping mechanics is crucial for several reasons:
Key Components of Proper Jumping Mechanics To ensure children are jumping safely and effectively, it's essential to focus on the following key components of jumping mechanics:
Red Flags: Signs of Improper Jumping Mechanics While observing children's jumping activities, keep an eye out for the following red flags, which may indicate improper jumping mechanics:
Proper jumping mechanics are essential for pediatric populations to jump safely, efficiently, and with minimal risk of injury. By focusing on key components such as knee bend, arm swing, soft landings, core stability, and foot alignment, children can develop healthy movement patterns and enjoy the benefits of jumping activities. Additionally, being aware of red flags indicating improper mechanics allows parents, coaches, and healthcare providers to intervene early and provide necessary guidance and support for children's physical development and well-being. So, let's encourage our young jumpers to LEAP into health with confidence and proper form!
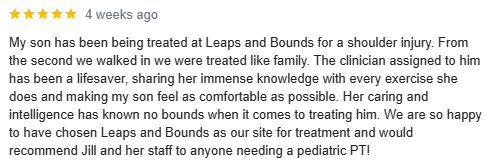
As we wave goodbye to another transformative chapter and eagerly embrace a new one, we're filled with deep gratitude and immense pride as we reflect on the incredible milestones and journeys that have enriched the story of Leaps and Bounds. The past year stands as a testament to our growth, joy, and unwavering dedication to empowering our patients to reach their utmost potential.Celebrating Patient Success Stories: Throughout the year, we've had the honor of witnessing remarkable transformations among our patients. From overcoming post-injury challenges to achieving newfound mobility, each success story represents the dedication of both our skilled therapists and the determination of our patients. Explore glimpses of these incredible journeys in our Google reviews and Instagram highlights! Click the Instagram icon above to follow us and see how our |
WelcomeWelcome to the Leaps and Bounds Blog page where you can find helpful parent information, tips and other topics of interest. Check back monthly for new entries and be sure to send us a message if there are any topics you'd like to learn more about! Archives
July 2024
Categories |
|
Insurance Based Pediatric Outpatient Rehabilitation
|
LOCATIONSSOUTH SHORE COMMONS
2955 Veterans Road West Staten Island, NY 10309 (718) 477-1911 RICHMOND AVENUE 1550 Richmond Avenue Staten Island, NY 10314 (718) 313-4743 NEW JERSEY 670 N. Beers Street (Unit 1) Holmdel, NJ 07733 (732) 479-2474 |
About Us Physical Therapy Services Schroth Treatment Dynamic Movement Intervention Continuing Education Join Our Team! Blog Contact Us © COPYRIGHT 2015. ALL RIGHTS RESERVED.
|